How to Treat Seborrheic Dermatitis on the Scalp: A Complete Guide
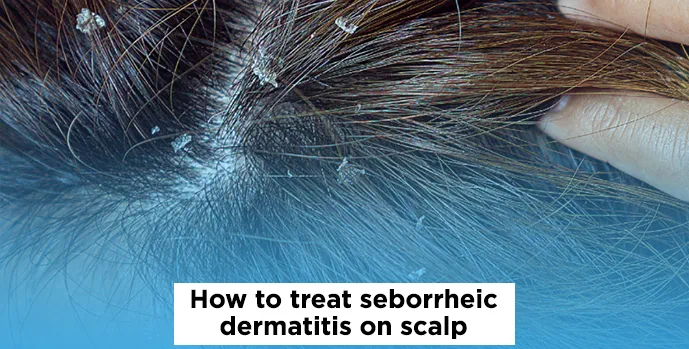
Seborrheic dermatitis on the scalp can be frustrating,itchy, flaky, and often persistent. Whether you're noticing greasy scales, red patches, or relentless dandruff, you're not alone. Many people search for effective ways to treat seborrheic dermatitis on the scalp and reduce flare-ups. Fortunately, with the right products and care routine, this condition can be managed successfully.
In this guide, we’ll walk you through the best treatments for seborrheic dermatitis on the scalp, covering everything from medicated shampoos to scalp care tips and dermatologist advice. If you're looking for a reliable and practical approach to soothe your scalp, read on.
What is Seborrheic Dermatitis on the Scalp?
Seborrheic dermatitis is a chronic inflammatory skin condition that mainly affects areas rich in oil glands—especially the scalp. It often appears as:
-
Flaky, white or yellowish scales
-
Greasy patches on the scalp
-
Redness or mild inflammation
-
Itching or discomfort.
The exact cause isn't fully understood, but factors like overactive sebaceous glands, Malassezia yeast overgrowth, and genetics may contribute. Although seborrheic dermatitis is not contagious or harmful, it can be cosmetically and physically bothersome.
Best Treatments for Seborrheic Dermatitis on the Scalp
Treating scalp seborrheic dermatitis involves a combination of medicated products, anti-inflammatory agents, and consistent scalp hygiene. Below are the most recommended methods:
1. Medicated Shampoos
The first and most important step is using medicated shampoos for seborrheic dermatitis. These shampoos contain active ingredients that help control yeast growth, reduce inflammation, and remove scaling. Key ingredients to look for:
-
Ketoconazole (2%) – Antifungal that targets Malassezia yeast.
-
Selenium Sulfide (1–2.5%) – Reduces scalp oiliness and fungal activity.
-
Zinc Pyrithione – Has both antifungal and antibacterial properties.
-
Coal Tar – Slows down skin cell production and reduces scaling.
-
Salicylic Acid – Helps remove flakes by exfoliating dead skin.
Popular products include Nizoral (ketoconazole-based), Head & Shoulders Clinical, and Selsun Blue (selenium-based). Medicated shampoos usage tips:
-
Use the shampoo 2–3 times a week initially, then reduce as symptoms improve.
-
Massage into the scalp and leave it on for 5–10 minutes before rinsing.
-
Alternate between 2 different shampoos to prevent resistance.
2. Topical Antifungal Creams or Lotions
For localized flare-ups or stubborn patches, topical antifungal treatments are effective. These usually contain:
-
Ketoconazole 2% cream or foam.
-
Ciclopirox.
-
Clotrimazole or Miconazole (OTC options).
These treatments are particularly helpful for areas like the hairline, behind the ears, or other patches not easily reached by shampoo. How to apply:
-
Clean the area and apply a thin layer to the scalp once or twice daily.
-
Avoid overuse to reduce the risk of resistance.
-
Can be used in conjunction with medicated shampoos.
3. Anti-Inflammatory Treatments
Sometimes, inflammation and redness may require more than antifungals. This is where mild corticosteroids or non-steroidal alternatives can help. Mild Corticosteroids (Short-Term Use):
-
Hydrocortisone 1% cream or lotion.
-
Betamethasone or Clobetasol (prescription options).
These reduce itching and redness quickly, but long-term use can thin the skin or cause resistance. Natural anti-inflammatory options:
-
Aloe Vera Gel – Soothing and cooling for inflamed areas.
-
Tea Tree Oil – Has antifungal and anti-inflammatory properties (dilute before use).
-
Apple Cider Vinegar Rinse – Balances scalp pH (mix 1:1 with water).
Scalp Care Tips to Support Treatment
Treating seborrheic dermatitis is not just about medications—your daily habits play a crucial role too. Here are essential scalp care practices:
Gentle Washing Routine
-
Avoid overwashing your hair, which can strip natural oils.
-
Use lukewarm water, not hot.
-
Gently pat dry your scalp instead of rubbing.
Avoid Harsh Hair Products
-
Steer clear of alcohol-heavy styling gels or sprays.
-
Use sulfate-free, fragrance-free shampoos on non-treatment days.
-
Avoid heavy oils or greasy conditioners that may worsen buildup.
Manage Your Triggers
Common triggers that can worsen seborrheic dermatitis include:
-
Stress – Practice relaxation techniques or yoga.
-
Cold, dry weather – Use a humidifier at home.
-
Poor diet – Eat a balanced diet rich in omega-3s and antioxidants.
A healthy scalp is more resilient to flare-ups. Making small lifestyle changes can complement your treatment strategy.
When to See a Dermatologist?
While most mild to moderate cases can be managed at home, some situations require medical attention:
-
Symptoms persist after 4–6 weeks of consistent treatment.
-
You develop painful, oozing, or infected patches.
-
Flare-ups become more frequent or intense.
-
You need guidance on prescription-strength antifungals or steroid alternatives.
A dermatologist can provide tailored treatment options, such as oral antifungals or immunomodulatory creams, if topical methods aren’t enough.
Final Thoughts:
The key to managing seborrheic dermatitis on the scalp is consistency. Whether you're using ketoconazole shampoo, antifungal creams, or anti-inflammatory agents, sticking to a regular scalp care routine is crucial.
Combine effective treatments with a gentle hair care regimen and lifestyle adjustments to keep flare-ups under control. If over-the-counter products aren't enough, consult a dermatologist for advanced Seborrheic Dermatitis Treatment solutions. With the right approach, living with seborrheic dermatitis becomes much more manageable, and your scalp will thank you for it.
Visit Skinfinity Derma Clinic.